Jo, Year 13, explores what is happening chemically inside the brains of those suffering from eating disorders and shows how important this science is to understanding these mental health conditions.
The definition of an eating disorder is any range of psychological disorders characterised by abnormal or disturbed eating habits. Anorexia is defined as a lack or loss of appetite for food and an emotional disorder characterised by an obsessive desire to lose weight by refusing to eat. Bulimia is defined as an emotional disorder characterised by a distorted body image and an obsessive desire to lose weight, in which bouts of extreme overeating are followed by fasting, self-induced vomiting or purging. Anorexia and bulimia are often chronic and relapsing disorders and anorexia has the highest death rate of any psychiatric disorder. Individuals with anorexia and bulimia are consistently characterised by perfectionism, obsessive-compulsiveness, and dysphoric mood.
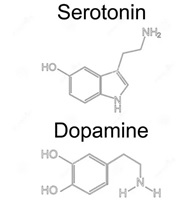
Dopamine and serotonin function are integral to both of these conditions; how does brain chemistry enable us to understand what causes anorexia and bulimia?
Dopamine
Dopamine is a compound present in the body as a neurotransmitter and is primarily responsible for pleasure and reward and in turn influences our motivation and attention. It has been implicated in the symptom pattern of individuals with anorexia, specifically related to the mechanisms of reinforcement and reward in engaging in anorexic behaviours, such as restricting food intake. Dysfunction of the dopamine system contributes to characteristic traits and behaviours of individuals with anorexia which includes compulsive exercise and pursuit of weight loss.
In people suffering from anorexia dopamine levels are stimulated by restricting to the point of starving. People feel ‘rewarded’ by severely reducing their calorie intake and in the early stages of anorexia the more dopamine that is released the more rewarded they feel and the more reinforced restricting behaviour becomes. Bulimia involves dopamine serving as the ‘reward’ and ‘feel good’ chemical released in the brain when overeating. Dopamine ‘rushes’ affect people with anorexia and bulimia, but for people with anorexia starving releases dopamine, whereas for people with bulimia binge eating releases dopamine.
Serotonin
Serotonin is responsible for feelings of happiness and calm – too much serotonin can produce anxiety, while too-little may result in feelings of sadness and depression. Evidence suggests that altered brain serotonin function contributes to dysregulation of appetite, mood, and impulse control in anorexia and bulimia. High levels of serotonin may result in heightened satiety, which means it is easier to feel full. Starvation and extreme weight loss decrease levels of serotonin in the brain. This results in temporary alleviation from negative feelings and emotional disturbance which reinforces anorexic symptoms.
Tryptophan is an essential amino acid found in the diet and is the precursor of serotonin, which means that it is the molecule required to make serotonin. Theoretically, binging behaviour is consistent with reduced serotonin function while anorexia is consistent with increased serotonin activity. So decreased tryptophan levels in the brain, and therefore decreased serotonin, increases bulimic urges.
Conclusions
Distorted body image is another key concept to understand when discussing eating disorders. The area of the brain known as the insula is important for appetite regulation and also interceptive awareness, which is the ability to perceive signals from the body like touch, pain, and hunger. Chemical dysfunction in the insula, a structure in the brain that integrates the mind and body, may lead to distorted body image, which is a key feature of anorexia. Some research suggests that some of the problems people with anorexia have regarding body image distortion can be related to alterations of interceptive awareness. This could explain why a person recovering from anorexia can draw a self-portrait of their body image that is typically 3x its actual size. Prolonged untreated symptoms appear to reinforce the chemical and structural abnormalities in the brains seen in those diagnosed with anorexia and bulimia.
Therefore, in order to not only understand and but also treat both anorexia and bulimia, it is central to look at the brain chemistry behind these disorders in order to better understand how to go about successfully treating them.
